An Analysis of State and Federal Telehealth Reforms During and Beyond Covid-19
- Share via Email: An%20Analysis%20of%20State%20and%20Federal%20Telehealth%20Reforms%20During%20and%20Beyond%20Covid-19
- Share via Facebook: An%20Analysis%20of%20State%20and%20Federal%20Telehealth%20Reforms%20During%20and%20Beyond%20Covid-19
- Share via Twitter: An%20Analysis%20of%20State%20and%20Federal%20Telehealth%20Reforms%20During%20and%20Beyond%20Covid-19
Authors
Key Points
Telehealth is vital to the future of health care in the U.S. It has the ability to solve many health care access issues, but regulatory restrictions greatly hinder its usefulness. These restrictions were practically thrown out the window during the pandemic in the name of access, which leaves you to wonder how many of these restrictions are necessary going forward.
Every state made changes to telehealth policies that allowed for greater flexibility in how patients and practitioners could interact, but these changes were not uniform across the country. For example, every state allowed patients to talk on the phone with their behavioral health professional for a consultation instead of meeting in person. Yet, only a few states allowed psychologists to provide virtual services across state lines without going through the typical licensing process.
Some states used the telehealth lessons learned during the pandemic as a springboard to make telehealth more accessible beyond the pandemic. But some are going back to business as usual, even as research shows patients and providers are pleased with the flexibility and accessibility that telehealth has provided. We will likely see greater variance in state telehealth landscapes as a result.
Media Contact
For general and media inquiries and to book our experts, please contact: [email protected]
Introduction
By March 17, 2020, most states had declared a state of emergency due to the spread of COVID-19, and governors began to issue executive orders aimed at controlling the spread of the virus. Stay-at-home orders, as well as concerns over surging COVID-19 cases and hospital capacity, made in-person visits for many health-related services, including preventative care, low-priority or entirely inaccessible. Due to this shift, state and federal leaders temporarily suspended many regulations that limited the use of telehealth in order to increase virtual access to health care. All 50 states and Washington, D.C. temporarily rolled back restrictions on telehealth to varying degrees. Many rollbacks will eventually or have already expired as states end their declared state of emergency, but some states are making permanent changes to telehealth policies.
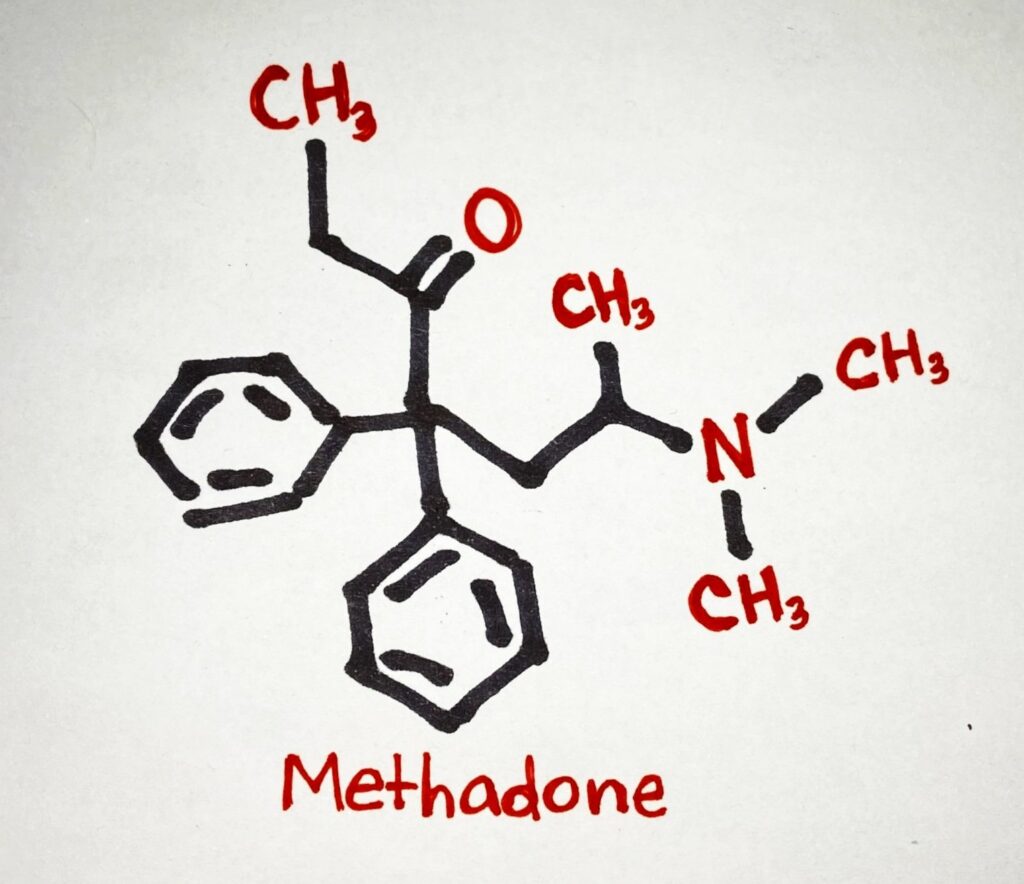
A somewhat murky but continuously evolving picture of telehealth regulation in the United States emerges amongst temporary executive orders, state of emergency extensions and expirations, state and federal government agency directives and numerous proposals to make permanent changes to various telehealth policies. This paper provides a brief overview of the changing trends in telehealth policies during the pandemic for four main categories of telehealth delivery mechanisms: audio-only, live video, store-and-forward and cross-state license policies. It also provides a snapshot of permanent telehealth changes made to expand the use of these delivery mechanisms beyond the pandemic. Finally, it will offer a few key policy recommendations for policymakers seeking to expand telehealth in their state.
Policy Recommendations & Infographics:
- Consider audio-only telehealth expansions. Audio-only telehealth became accessible in all 50 states and Washington, D.C. during the pandemic. Now, as evidence emerges on where audio-only telehealth is most useful–particularly for rural and low-income areas without broadband access–policymakers should consider which pandemic-era audio-only policies helped these communities the most, and ensure state regulations allow for them.
- Make specific allowances for store-and-forward telehealth to take better advantage of its full potential. Especially in states with rural and remote communities, store-and-forward telehealth can greatly complement synchronous telehealth and traditional in-person care. For urban areas, store-and-forward telehealth provides greater convenience and flexibility for patients and physicians alike and eases the need of taking time for appointments. Thus, more states should move towards legislation that reimburses store-and-forward telehealth. To do this, patients, physicians and legislators must be assured that asynchronous telehealth is a safe modality that can protect a patient’s personal information, and is a sufficient means through which a patient-physician relationship can be established.
- Enhance flexibility for patients and providers located in different states. Telehealth facilitates the connection between patients and providers regardless of the geographic distance, but states are slow to adopt permanent cross-state licensing reforms with the same regularity as audio-only methods. Policymakers looking to expand telehealth should consider state restrictions on medical licenses, and look to join licensure compacts or eliminate in-state license requirements.
Made with Visme
Made with Visme
Made with Visme
Made with Visme
Made with Visme
Made with Visme
Made with Visme
Made with Visme
Made with Visme
Made with Visme
Made with Visme
Made with Visme
Made with Visme