Pharmacy Access to Birth Control: Lessons From New Mexico
Summary
Many methods of hormonal contraception are unnecessarily put behind a prescription barrier at a doctor’s office or clinic, and many women have trouble regularly obtaining preferred methods. Pharmacies, on the other hand, can be more accessible than doctor’s offices, and patients in rural regions can particularly benefit from increased pharmacy access to birth control. Nearly 90 percent of Americans live within 5 miles of a pharmacy. The pharmacy access model, in which pharmacists can prescribe/furnish most hormonal birth control methods directly to patients, is a mechanism states use to lower barriers to contraception.
States have increasingly adopted the pharmacy access model—almost half of all states now allow it. Now that it has gained traction, it is important to examine whether pharmacists and pharmacies are taking the required steps to offer birth control consultations, and if not, the reasons why. This can help guide efforts to bolster pharmacist participation in contraception prescribing.
Pharmacy Access Uptake: A Look at New Mexico
To explore pharmacy access uptake, we conducted a survey of select New Mexico pharmacies to learn how many pharmacists are certified to prescribe birth control and how often patients request consultations.
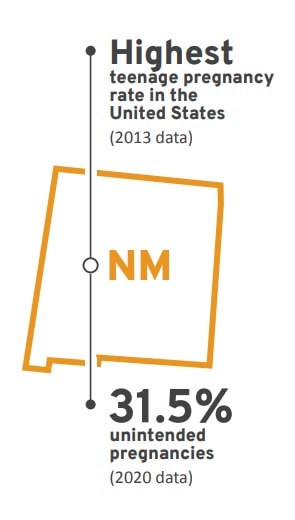
We chose New Mexico for several reasons. First, New Mexico was one of the first states to implement this model. Second, New Mexico generally adheres to best practices for pharmacy access: the state has no patient age restriction, all forms of self-administered hormonal contraception can be prescribed by pharmacists, and pharmacist-initiated prescriptions for birth control are covered through insurance. Finally, New Mexico lacks primary care and reproductive health access: New Mexico had the highest teenage pregnancy rate in the United States in the most recent data, and nearly a third of pregnancies in New Mexico were unintended as of 2020. All of these factors increase both patient and pharmacist incentives to take advantage of pharmacy access.
Pharmacy Access Activity Across New Mexico
The survey spanned 106 pharmacies throughout New Mexico, both independent and chains, excluding most national chains (CVS, Walgreens and Walmart). These national chains were excluded since each has a corporate policy on pharmacists prescribing, so survey outreach was unnecessary. Each pharmacist was asked whether they or any pharmacist at their location was able to prescribe birth control. If yes, a broad estimation of patient use was requested as was an urban-rural classification for the pharmacy’s location. If no pharmacist was able to prescribe birth control, we asked whether they would cite a specific reason for not providing this service.
Of the pharmacies called, 71 percent responded (75 pharmacies total). Of all pharmacists reached, all were aware of the statewide order authorizing them to prescribe birth control after completing certain education requirements.
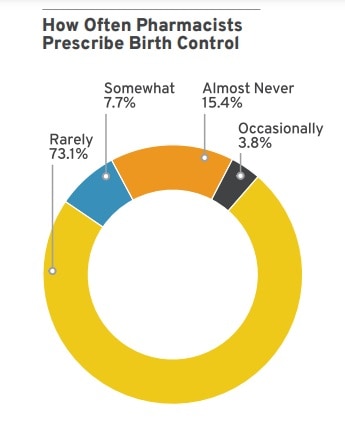
Twenty-six pharmacies had at least one pharmacist on staff eligible to prescribe birth control. Of these, the majority (73 percent) state that they only do so rarely, between zero-to-two times per month. Fifteen percent of pharmacists prescribe fewer than three times per year, and 10 percent prescribe more often, with approximately two or more prescriptions per month.
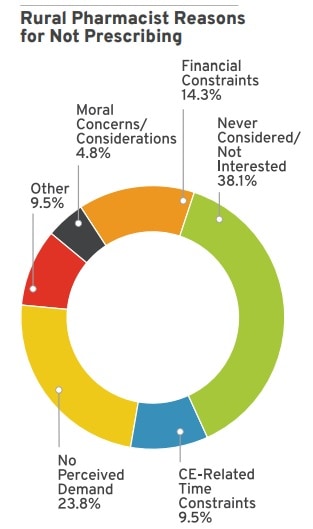
Sixty-five percent of all pharmacies reached do not have any pharmacist that prescribes birth control. Over 30 percent of pharmacists who do not prescribe birth control listed a general lack of interest or incentive to complete the continuing education (CE) requirements and generate or uphold their status as contraception providers. The next most cited reason (24 percent) was that they felt there was no community demand, followed (10.8 percent) by time constraints associated with CE that made the courses not worthwhile.
Breaking down the responses by urban-rural classifications also yielded noteworthy results. The most commonly cited reason for not prescribing birth control among self-defined rural pharmacies was a lack of general consideration of the practice, whereas a lack of demand was more common for urban pharmacists. Overall, rural pharmacies were less likely to prescribe birth control.
Translating Survey Results into Action
There are three primary takeaways from the survey results. If pharmacist participation in prescribing is relatively low but the statewide order follows best practices, then the issue is beyond writing better rules. First, it is likely patients are unaware of the pharmacy access model and therefore do not ask pharmacists for prescriptions. Other states have also faced this issue, with middling efforts to solve the problem. Second, for pharmacists that did not have time to complete required trainings, it is likely that having too many other primary duties to fulfill prevent participation. This is a nationwide issue that speaks to a larger primary care shortage. Finally, pharmacists in rural locations may benefit from further incentive or awareness campaigns about the value of offering birth control prescribing. New Mexico can address all of these issues with an initiative similar to a recent one focused on contraceptive access and awareness in the state.
Contact us
For more information, please contact:
Courtney Joslin
Resident Fellow and Senior Manager
Competition Policy
cjoslin@rstreet.org
Sophia Heimowitz
Research Assistant
Competition Policy
sheimowitz@rstreet.org
MEDIA CONTACT
For general media inquiries and to book our experts, please contact pr@rstreet.org.

